What happens during a root canal?
Root canal therapy (RCT) is necessary to save a tooth with infected or inflamed pulp (sometimes called the “nerve” of the tooth).
Endodontics, also known as endodontology, is the dental speciality that deals with root canal therapy. The Dental Board of Australia recognises endodontics as a speciality and keeps a registry of specialist endodontists who have completed at least three years of advanced education in the field.
When a tooth’s pulp becomes inflamed or necrotic (dies), endodontic therapy is necessary. Abscesses can develop when a dead nerve is present. Trauma, such as a blow to the mouth or tooth, severe dental disease (dental caries), a crack or break in the tooth, or even a reaction to a very deep filling or the insertion of a new crown on a damaged tooth can induce inflammation of the pulp, or even pulp deaths.
Pain and swelling are common initial symptoms of an endodontic problem, however in many situations the patient may have no discomfort prior to the diagnosis of an endodontic issue via a routine radiograph.
Over the course of one or two visits, an endodontist or general dentist will drill a small hole in the crown of the tooth and remove the infected or diseased pulp using a series of fine files. Once the canals have been prepared for filling, a powerful antibacterial solution is used to ensure that all germs are killed before the procedure begins.
After the root canals have been irrigated with an antibacterial solution, they are dried using tiny sterile paper cones and filled with a pliable rubbery material.
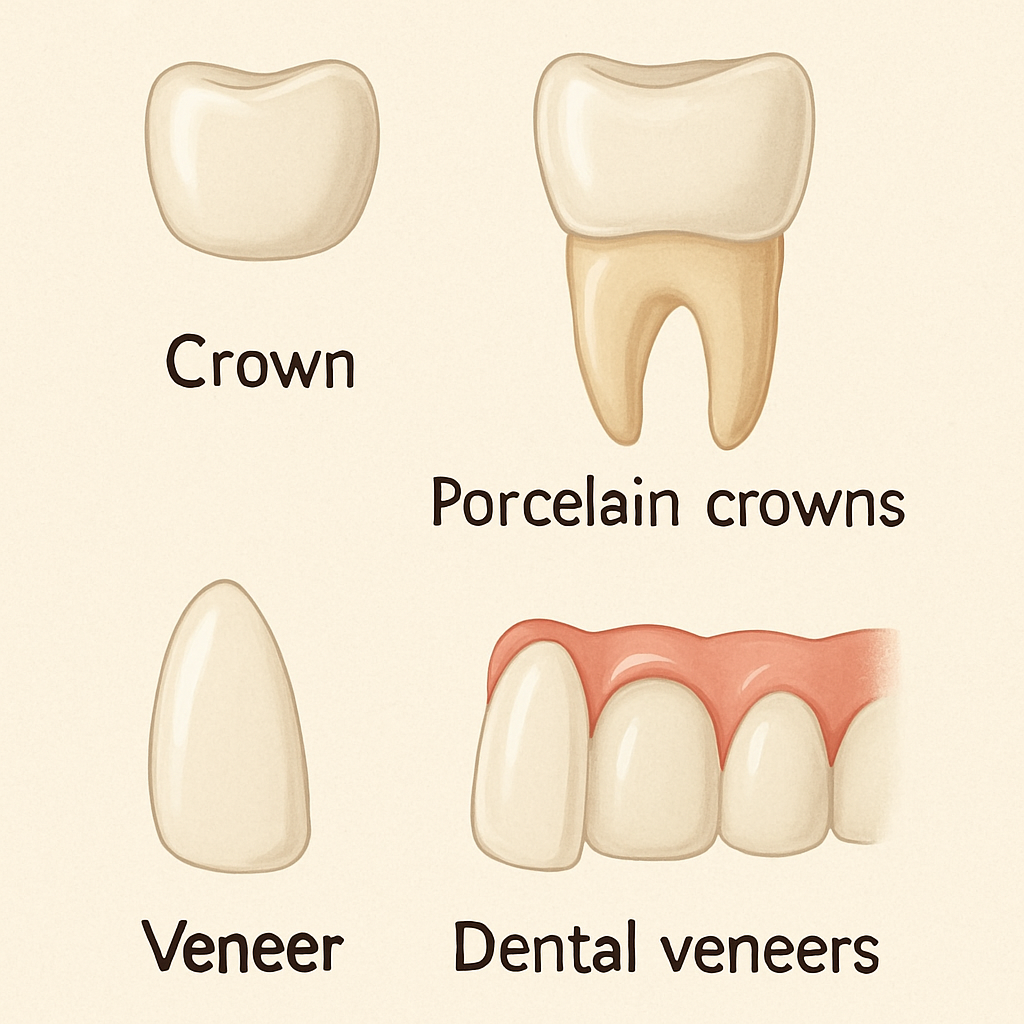
An irreversible restoration is placed as the final step in the treatment of a root-filled tooth. Sometimes all that’s needed is a filling, but more often it takes a crown or some other elaborate restoration.
Since local anaesthetic is utilised during the entire procedure, root canal therapy shouldn’t cause any discomfort.
The majority of patients report mild to moderate discomfort after surgery, which is easily managed with pain relievers for a day or two.
As with any endodontic procedure, the success rate of RCT performed by an endodontist is high, and the outcome can be predicted with reasonable accuracy.
Who can administer the required care?
A general dentist can perform root canal therapy if necessary. Because of the complexity of this treatment, however, it is usually recommended that you see an endodontist instead.
The dentists in Australia who specialise in endodontics have earned a Master’s or a Doctorate in the area, during which time they have conducted original research and honed their practical skills in the administration of complex root canal treatments. As was previously indicated, they must be registered with the Dental Board of Australia and are subject to tight regulation.
After endodontic therapy, your regular dentist or a prosthodontist (a restoration specialist) will make any necessary cosmetic adjustments to your teeth.
What is the estimated price tag for care?
Costing around $150, a visit to an endodontist’s office doesn’t require a doctor’s recommendation (but one is accepted).
Endodontic treatment can cost anywhere from $1,700 to $2,700, with a subsequent filling costing between $200 and $450.
Is it uncomfortable to get a root canal?
Before anaesthetics were widely available, root canal therapy may be quite a frightening ordeal for the patient. Therefore, ever then, root canal therapy has been stigmatised.
However, because to scientific discoveries and medical progress, this type of treatment is now considered to be non-traumatic. Modern root canal procedures cause so little discomfort that many patients nod off during the procedure, and some even use a little rubber bite block to rest their jaws on so they don’t have to keep their mouth open consciously the whole time.
Even after the area has been numbed, most patients report feeling a combination of pressing, pulling, pressure, and vibration during modern root canal therapy. These feelings are typical and to be expected.
Acute discomfort is not typical, however. Because anaesthetic doses and the procedures needed to achieve total numbness differ between persons, disease stages, tooth kinds, and tooth locations, patients are encouraged to communicate any discomfort they experience during treatment with their doctor. During the course of your therapy, your doctor may need to make a few alterations to ensure your comfort.
Even if current anaesthetics are effective in reducing the body’s physical response to pain, they do little to alleviate the emotional suffering that often accompanies it. Anxious and tense patients may have trouble with pain medication and may require additional measures to alleviate their suffering. If a patient is affected, they should inform their doctor during the initial visit so that they can take the necessary precautions.
How can I improve my level of comfort during this necessary root canal procedure?
Typically, your endodontist will begin treatment by focusing on the emotional side of any pain you may be experiencing. So that you are prepared emotionally, they will explain what they plan to do and how you will likely react. They’ll also reassure you that you’re free to end therapy whenever you like.
Eighty percent to ninety percent of patients only require this form of comfort on a mental level. If it isn’t enough, though, your endodontist will likely prescribe anxiety medication to be taken before the procedure. If that isn’t enough, you may always add some happy gas (nitrous oxide) to your regular anaesthetic for a more relaxing and comfortable experience.
You can see that there are a variety of methods that professionals can use to make root canal therapy more tolerable for you. Your degree of anxiety, among other things, will be discussed during your appointment to help determine which treatment strategy will be most effective for you.
Don’t be shy about addressing your worries with your healthcare provider. Thus, they can make your endodontic procedure as painless as possible.
Root canal treatment vs. tooth extraction and implant: what are the benefits?
Root canal treatment and tooth extraction and implant are like natural limbs and prosthetics, respectively.
When assessing the relative benefits of different treatments, the myths unfortunately tend to drown out the realities. It is my hope that by elucidating some of these common misunderstandings, I might help you gain a deeper appreciation for this topic.
The first false belief is that getting an implant is preferable since “I will have to have one later anyhow.”
The success rate of root canal treatment and dental implants can be comparable. That means each should have a lifespan of at least 15–20 years. An implant can be used as a backup option in case a tooth that has had a root canal treatment fails to recover. If an implant fails, the success rate of subsequent implants decreases. There are no permanent things in this world. By preserving your natural teeth for as long as possible (through root canal therapy), you can put off getting implants for a while longer. This means that the tooth in question can be handled and kept for longer.
Second Fallacy: “Dental implant success rates are comparable to those of root-canal treated teeth.”
Potentially, yes.
Once the validity of each study is examined, a trend emerges. There is a dividing line between a successful root canal treatment (no disease) and an unsuccessful one (evidence of disease). When discussing dental implants, the terms “success” (implant retention without disease) and “retention” are frequently used interchangeably (meaning the implant may still be in the mouth despite having disease, which does not equate to success). This basic fact is frequently twisted to make implants seem alluring. Therefore, it is important to be cautious about the information you take from the web.
Many host factors, including the implant’s location, bone quality, immune system, gum health, smoking history, and medications, can affect the implant’s likelihood of success. The odds of a successful root canal treatment are much higher and there are less obstacles.
When considering getting implants, age is also important. The human body can usually keep growing until at least the age of 25. If eruption and jaw development continue after an implant has been put, the implant’s cosmetic appearance may suffer.
Finally, it can be more tough to make a dental implant look as “natural” as an actual tooth.
Third Fallacy: “Because it’s new, implant technology must be an improved treatment.”
That’s not always the case. One should not automatically assume that something brand new is superior. Due to its long history of use, root canal therapy is one of the most studied dental procedures. Only since the latter part of the twentieth century have we had implant technology, and even now, as more and more long-term data becomes accessible, we doctors are continually honing this technology.
No. 4: “An implant would be as expensive as root canal therapy.”
No. Root canal therapy is typically less expensive than tooth extraction and implant placement. However, if a crown is needed to safeguard a weak or decayed back tooth, the treatment cost can be close to that of a normal front tooth.
False Belief No. 5: “I had a root canal and it didn’t work.”
The loss of one tooth does not necessarily indicate the need to replace the rest. Root canal therapy is a sensitive procedure, the success of which is reliant on the practitioner’s expertise. The location, size of the filling, and severity of the infection might also vary from tooth to tooth within the same mouth.
If dentists had to choose between getting a root canal and having a tooth extracted, which would they pick?
Most dentists would rather have a root canal done on one of their own teeth (figuratively speaking) than obtain an implant. What more can be said?
After getting a root canal, what should I anticipate?
Restoration with a crown or comparable tooth restoration is typically recommended after therapy to safeguard the weakened tooth and forestall further cracking or fracturing.
Any tooth that a root canal specialist saves will likely continue to operate normally for a very long time. When a tooth has deteriorated to the point that even root canal therapy won’t save it, it’s usually because of decay, wear, or trauma. Consequently, root canal therapy does not always produce the desired outcome. A few examples are as follows:
root fractures that necessitate extraction of the tooth; post-treatment sensitivity or pain from the trauma of treatment or occlusion (or biting) effects; residual infection due to inability to effectively remove all the “nerve” tissue due to complexity of the root canal system (e.g. curved roots, accessory canals, additional canals); It’s possible for there to be leakage of substances into the neighbouring tissue.
However, complications such as infection or a fractured root or tooth can arise at a later period and require the removal of the affected tooth. To avoid the need for future tooth extraction, an implant-supported tooth is sometimes the best alternative.